(Note: if you are reading this via email notification, do NOT reply to the email if you want to comment. Click on the title of the blog post, which will take you directly to the blog post. Scroll down to comment there.)
******************************************
 Dear STTM Blog readers, I am so fortunate to talk to many wonderful individuals because of Stop the Thyroid Madness. And recently, I had a conversion with the very insightful Dr. Hugh Melnick of New York City.
Dear STTM Blog readers, I am so fortunate to talk to many wonderful individuals because of Stop the Thyroid Madness. And recently, I had a conversion with the very insightful Dr. Hugh Melnick of New York City.
Dr. Melnick brought my attention to a very disturbing article titled “For borderline underactive thyroid, drug therapy isn’t always necessary” that came from the Harvard Health Letters in October 2013, You can see it here: http://www.health.harvard.edu/blog/for-borderline-underactive-thyroid-drug-therapy-isnt-always-necessary-201310096740.
This conversation between Dr. Melnick and I may be of great interest to STTM readers, besides alarming once you see what is being stated in this article and suggested as treatment guidelines. It’s simply Thyroid Treatment Dark Ages!
*****
JANIE:Â Hello Dr. Melnick. I’m so glad to chat with you! Can you tell our readers a little about yourself?
DR. MELNICK: I am a reproductive endocrinologist who has been in medical practice since 1976. As the medical director of Advanced Fertility Services In Vitro Fertilization Center in New York City, I have always been impressed by the large number of infertile women that I have seen over the years, who are symptomatically hypothyroid, and who conceive after treatment with thyroid medication.
Although I did my medical training at a point in time when the TSH test and Synthroid were just being introduced into clinical practice, I was trained by one of the most widely respected endocrinologists of that era, Herbert Kupperman, MD, Ph.D. to diagnose and treat patients with potential thyroid issues according to their symptoms, rather than solely by their blood test results. His vast clinical experience, and subsequently mine, as well, is that treatment with Natural Desiccated Thyroid (NDT) gives far superior symptomatic improvement for the vast majority of patients. Furthermore, the dosage of thyroid medication should always be based upon a patient’s clinical symptoms and not the TSH level.
JANIE: That greatly impresses me when I learn of doctors like yourself who understand the efficacy of Natural Desiccated Thyroid as well as the problems with using the TSH lab test. Â You recently brought my attention to what was written just a few months ago by Heidi Godman, the Executive Editor of Harvard Health Letter (see introduction above). Can you expound on what Ms Godman meant by “borderline underactive thyroid”?Â
DR. MELNICK:Â Actually, Ms. Godman is mistakenly defining hypothyroidism by TSH levels, rather than by a patient’s clinical symptoms. It is obvious that there are many symptomatic and genuinely hypothyroid individuals, who have normal TSH levels, and who experience relief when given a proper dose of the appropriate thyroid medication. The TSH level only diagnoses a type of hypothyroidism that is due to failure of the thyroid gland itself, or a failure of the pituitary gland.
In my experience, the most common form of hypothyroidism is called subclinical because the TSH levels are in the “normal range.” It is a genetic condition, usually passed through the mother and manifests itself later in adulthood. In subclinical hypothyroidism, the individual’s cells need more active thyroid hormone–T3–than their bodies are able to produce in order to function properly. Therefore, supplementation with a thyroid medication containing T3, in the proper dose, will relieve the troubling symptoms and allow the cells to function optimally.
Again, basing the dosage of thyroid medication on TSH levels is incorrect. When treating hypothyroidism, we are not treating a condition like diabetes, in which the insulin dose is based upon the patients’ blood sugar levels. Although they are both endocrine disorders, they are vastly different conditions and cannot be treated in the same fashion, although many endocrinologists still insist on doing so!
JANIE: In the article, Godman quotes that prescriptions for levothyroxine have increased from 50 million in 2006 to about 70 million in 2010, and a similar increase has occurred in England and Wales. She then calls this increase in treatment “pretty risky business”, citing irregular heart rhythms, insomnia, and loss of bone density”. What is she implying there?
DR. MELNICK: I think that the observed increase in the use of the thyroid medication Synthroid is due to the fact that hypothyroidism is a very common condition, affecting at least 35% of the female and 10% male population. Considering the population estimates for 2013 is 317 million people in the U.S.A. and the population of the United Kingdom is estimated to be 70 million, 28% of the population in the U.S. and 23% of the population in England, (assuming one prescription per year per individual patient) are being treated for hypothyroidism. This is actually a bit less than the estimated incidence of hypothyroidism in this country. I also believe that more cases of hypothyroidism are being found because people, in general, are more informed about the symptoms of hypothyroidism and seek treatment.
In my opinion, Ms. Godman erroneously categorizes treatment of hypothyroidism a “pretty risky risky business”. The risks of not treating hypothyroidism is, in fact, more potentially injurious to a patient’s health!Â
For example, the increased risk of heart disease in untreated hypothyroid individuals is a solid example of why hypothyroidism needs to be treated. The examples that she cites, namely, irregular heart rhythms and insomnia, are found in many people with hypothyroidism before treatment and are cured by adequate thyroid treatment. The symptoms that she mentioned are not exclusively associated with hyperthyroidism. The loss of bone density claim comes from studies of hyperthyroid individuals, who because of their hyperthyroidism and excessively high metabolic rate, may develop osteoporosis.
JANIE: The next part of this article is alarming. It refers to a particular “clinical practice guidelines” authored by Endocrinologist Dr. Jeffrey Garber, an associate professor of medicine at Harvard Medical School. These guidelines come from a task force representing the American Thyroid Association and the American Association of Clinical Endocrinologists. The first guideline is as follows, and goes completely against what informed thyroid patients know to be wise. Can you comment?Â
1) The best way to check for hypothyroidism is to look at the level of thyroid stimulating hormone (TSH) in the blood, and when the TSH level is above 10 mIU/L, there’s uniform agreement that treatment with levothyroxine is appropriate.Â
DR. MELNICK:Â Firstly, clinical practice guidelines are merely suggestions that have been developed to help physicians with limited experience diagnose and treat medical issues. Clinical guidelines are like a cook book, which describes a recipe that makes a simple meal, but not necessarily a complex and elaborate feast. That said, it is quite obvious that the way in which I diagnose and treat hypothyroidism is quite different than that which is suggested by the above referenced societies.
Although I do perform a complete battery of blood tests, including antithyroid antibodies, iron, vitamin B12 and vitamin D levels, I believe that a clinical approach – listening to a patient’s symptoms and treating a patient accordingly – is, in some ways, more important in diagnosing and properly treating patients suffering with the symptoms of hypothyroidism. If a physician only looks at a patient’s blood tests, without listening to the patient’s symptoms and asking them appropriate questions, many people who legitimately need thyroid medication will be denied proper treatment. That is precisely the reason that so many people come to me suffering with all the classical symptoms of hypothyroidism and tell me that their doctors have tested their thyroid and found them to be “within normal limits”.
It is not surprising when these very same patients experience symptomatic improvement when treated with adequate doses of NDT. I rarely treat patients initially with Synthroid. The primary reason is that Synthroid, being a synthetic T4 (a weak thyroid hormone- not chemically identical to human T4), must be converted into T3, the potent form of the hormone that enters every cell in the body and makes the cells of the body function normally. Unfortunately, many individuals are unable to successfully convert T4 into T3, so the patients’ symptoms remain, yet the TSH level is normal.
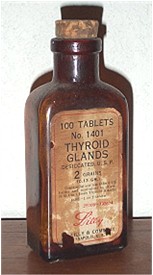
Natural desiccated thyroid (NDT) is made from the thyroid glands of pigs, which produce thyroid hormones chemically similar to that found in humans and does contain T3. Porcine (pig) thyroid gland also contains other thyroid hormones and proteins, which, in my experience are much more effective in relieving the symptoms of hypothyroidism than synthetic T4. Who can argue that a natural treatment, if availble, is to be preferred over a synthetic one.
JANIE: I loved the analogy above to a cook book, Dr. Melnick! Garber’s second most-emphasized guideline is the following, and I would love for you to comment on this as well, as informed thyroid patients would find this very disturbing, as well:Â
2)Â If the TSH level is between 4mIU/L and 10mIU/L, treatment may still be warranted in various situations: Â
- if the levels of actual thyroid hormones in the blood–known as thyroxine (T4) and triiodothyronine (T3)–are abnormal
- if the bloodstream contains anti-thyroid antibodies that attack the thyroid. These antibodies would indicate a hypothyroid condition called Hashimoto’s disease, in which the immune system mistakenly attacks the thyroid.
- if there is evidence of heart disease or risk for it.Â
Garber is next quoted as saying “Use thyroid hormone for a brief period of time.”  and “If you feel better, you can continue with treatment. If not, then stop.”  That recommendation is quite alarming as well, as it fails to understand that it may not be about stopping thyroid medication, but moving over to a far better treatment with natural desiccated thyroid, which informed thyroid patients know should have been the first treatment of choice anyway. Can you comment?Â
DR. MELNICK:Â In my clinical experience, 99% of patients with TSH levels over 4.0 are quite symptomatic, if questioned about their symptoms properly. Therefore, treatment is absolutely mandatory, both to relieve “quality of life symptoms” as well as to prevent heart disease, lower blood pressure, normalize blood sugar and cholesterol levels, if they are found to be elevated.
Dr. Garber’s recommendations about using thyroid medicine for a short period of time and continuing it if improvement is noted omits two essential factors. The first is that since he treats his patients only with Synthroid, a significant percentage will show no improvement because their symptoms are not relieved because they cannot convert T4 into T3. The second factor is that by following TSH levels in the blood, a patient may not actually be taking a high enough dose of thyroid medication, yet will show low TSH levels in the blood. The level of thyroid hormones circulating in the blood-whether they are bound or free- only indicate absorption of the medication and give no indication as to the amount of T3 entering the cells. When an individual gets enough T3 into their cells, their symptoms will improve.
The only way to measure the correct dose of thyroid medication, in addition to noting improvement in symptoms, is by measuring the Basal Body Temperature and by the measurement of nerve conduction velocity (Thyroflex Test). This is a noninvasive test which gives a good indication of dosage adequacy. The slower the patient’s nerve conduction velocity, the higher the dose of thyroid medication that is required.
One main point that must be noted is that thyroid medicine may take up to twelve weeks in order to experience some degree of symptomatic relief. The other is that the patients’ dosage should be increased gradually and in divided daily doses until symptomatic relief is experienced. The dose should be reduced if the patient experiences rapid or irregular heartbeat, shakiness or anxiety. These symptoms will resolve in several hours and are not harmful.
Hashimoto’s or autoimmune thyroiditis is a much more complex clinical condition, in that symptoms in many individuals may vary, from hypo to hyper from time to time. Treatment with thyroid hormone is usually needed, but some patients, in the early stages of thyroid autoimmunity, may be fairly asymptomatic. As the condition progresses, symptoms will eventually be experienced. The levels of antithyroid antibodies do not correlate with the severity of a person’s symptoms. Antithyroid antibodies never disappear and will always be detectable in the blood. There may also be gluten sensitivity in some instances, so dietary factors may be important. When an infertility patient is found to have antithyroid antibodies, whether they are symptomatic or not, I always treat them with NDT since it does help them to conceive and seems to reduce the incidence of miscarriages.
JANIE:Â Heidi Godman then states the following about individualized treatment for hypothyroidism, which informed thyroid patients know by years of experience is a recipe for disaster: “That requires measuring TSH four to eight weeks after starting treatment or changing a dose, another TSH test after six months, then every 12 months.” Â
DR. MELNICK: I respectfully disagree with both Ms. Godman’s formula as stated above, as well as with Dr. Garber’s method for diagnosing and treating hypothyroidism. Although the Harvard Medical School is a very prestigious institution, and that the information that they published cited the work of a physician of professorial rank, it is quite contrary to my own clinical experience and that of the many untreated or inadequately treated individuals who suffer with the many debilitating and disturbing symptoms arising from thyroid hormone deficiency.
I say this in jest, but if a patient follows the treatment protocol advocated by Ms. Godwon, they are more like to die of old age before their symptoms of hypothyroidism begin to show signs of clinical improvement .
JANIE: Your last sentence was excellent, Dr. Melnick. Your sage observations and wisdom jive with over a decade of successful patient experiences and wisdom! And we must push AGAINST the guidelines suggested by Dr. Jeffrey Garber. Informed thyroid patients know how disastrous they can be!
********************
**To sign up for email notifications of the STTM blog post, see bottom right of this page: //www.stopthethyroidmadness.comÂ
**To order your own labwork, go to the Recommended Labwork page.
 The following Guest Blog Post is written by Jill, who has a B.S. in Combined Sciences and is the mother six, including 22-month-old Moriah, a thyroid and adrenal patient who has Down syndrome.
The following Guest Blog Post is written by Jill, who has a B.S. in Combined Sciences and is the mother six, including 22-month-old Moriah, a thyroid and adrenal patient who has Down syndrome.